Understanding Uterine Fibroids: A South African Perspective
So, you've heard about uterine fibroids (non-cancerous growths in the womb)? Many South African women experience them, and understanding your options is key. This isn't just medical jargon; we'll explain fibroids clearly, discuss how they might affect you, and outline your treatment choices – from medication to surgery. We'll also share real-world experiences and practical tips to empower you to take control.
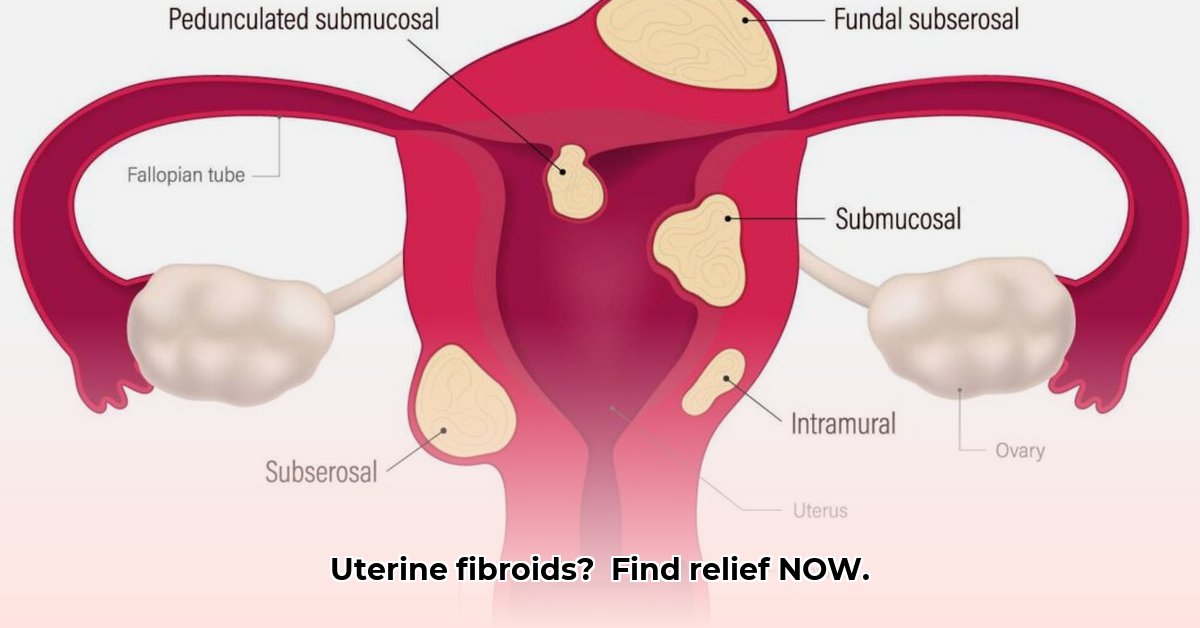
What are Uterine Fibroids?
Uterine fibroids are benign (non-cancerous) tumours that develop in the uterus. They're made of muscle tissue and are surprisingly common, particularly during a woman's reproductive years. Many women have fibroids without even knowing it! Why some develop them and others don't remains unclear, but hormones like estrogen and progesterone play a significant role, often explaining their appearance during childbearing years and shrinkage after menopause.
What Causes Fibroids?
While the exact cause remains a medical mystery, hormones definitely play a key role. Estrogen and progesterone, vital for menstruation and pregnancy, seem to fuel fibroid growth. This is why they often appear during your childbearing years and tend to shrink after menopause when hormone levels decrease. Remember, however, many women live their entire lives without ever developing fibroids.
Recognizing Fibroid Symptoms
Many women with fibroids experience no symptoms. However, for those who do, common signs include:
- Heavy menstrual bleeding (menorrhagia): Heavier and longer periods, requiring more sanitary protection.
- Pelvic pain or pressure: A constant ache or feeling of fullness in the lower abdomen.
- Frequent urination: Increased need to go to the toilet.
- Constipation: Difficulty with bowel movements.
- Painful intercourse (dyspareunia): Discomfort during sex.
Symptom severity varies greatly depending on fibroid size, location, and number. Some women experience mild discomfort, while others face significant disruptions to their daily lives.
Getting a Diagnosis: What to Expect
If you experience any of these symptoms, it's crucial to consult a gynaecologist or doctor. A pelvic exam is usually the first step, followed by imaging tests to confirm the diagnosis and assess fibroid size and location:
- Ultrasound: A painless procedure using sound waves to create images of your uterus.
- MRI (Magnetic Resonance Imaging): Provides even more detailed images.
- Hysteroscopy: A procedure to allow a closer visual examination of the uterus.
Treatment Options: Tailoring your Plan
Treatment choices depend on several factors: your symptoms, their severity, your desire for future pregnancies, and your overall health. Options include:
Medication: Medications like painkillers or hormonal therapies can manage heavy bleeding or pain. These don't cure fibroids but can alleviate symptoms. Remember, any medication should be prescribed by your doctor.
Myomectomy (surgical fibroid removal): This procedure removes the fibroids while preserving the uterus, leaving your fertility options open. However, it requires surgery with associated recovery time and risks.
Uterine Fibroid Embolization (UFE): A minimally invasive procedure blocking blood supply to the fibroids, causing them to shrink. Recovery is often quicker than myomectomy, but potential risks, like infection and pain, need discussion with your healthcare provider.
Hysterectomy (uterus removal): A last resort usually considered only if other treatments fail or if you no longer wish to have children. This is a major surgery with a longer recovery period and permanent infertility.
Important: This information is for general knowledge only. Always discuss your individual needs with your doctor to determine the best course of action. Regular check-ups are key to early diagnosis and management.
Best Minimally Invasive Surgery for Uterine Fibroids: A Personalized Approach
Key Takeaways:
- Minimally invasive surgeries offer effective alternatives to hysterectomy, often preserving fertility.
- The best procedure depends on factors like fibroid size, location, your age, and future pregnancy plans.
- Several minimally invasive options exist, each with unique benefits and drawbacks.
- Open communication with your gynaecologist is crucial for choosing the right approach.
- Pre-operative medication can sometimes enhance the effectiveness of other procedures.
Minimally Invasive Procedures: A Closer Look
While hysterectomy was once the primary treatment, minimally invasive techniques now offer less invasive options. These include:
Myomectomy: Surgically removing fibroids while preserving the uterus. Ideal for women wanting to maintain fertility, but it's more invasive than other methods, meaning a longer recovery time.
Uterine Fibroid Embolization (UFE): Blocking the blood supply to fibroids, making them shrink. It's less invasive than myomectomy, with a faster recovery, but with potential risks specific to the procedure.
Radiofrequency Ablation (RFA): Using heat to destroy fibroid tissue; minimally invasive and usually requiring a shorter recovery period. However, it may not be suitable for all fibroid sizes and locations.
MRI-guided Focused Ultrasound Surgery (MRgFUS): A non-invasive technique using focused ultrasound waves to destroy fibroids. It requires precise targeting and specific fibroid characteristics for optimal results.
Choosing the Right Path: Individualized Care
The best approach for you depends on various factors: your gynaecologist will evaluate:
- Fibroid size and location
- Your age and desire for future children
- Your overall health
- Your personal preferences and concerns
Your gynaecologist will help you weigh the benefits and risks of each approach to make an informed decision.
The Role of Pre-operative Medication
Before surgery, discuss with your doctor the possibility of pre-operative medication. Certain medications can help manage symptoms like heavy bleeding, possibly improving the success of other procedures.
Weighing the Risks: Informed Decisions
Minimally invasive procedures carry risks, such as bleeding, infection, organ damage, and nerve damage. While risks are generally low, you must discuss these possibilities with your healthcare provider. They can provide you with a tailored risk assessment.
Remember, navigating uterine fibroids can be challenging, but you don't have to face it alone. Open communication with your doctor and a comprehensive understanding of the available options will empower you to make the best decision for your health. Don't hesitate to ask questions; your well-being is paramount.